Chronic pain is one of the most misunderstood health issues today. While many people believe pain is only the result of an injury or disease, science has shown us that the nervous system itself can amplify pain signals, making you feel worse than the underlying condition may actually be.
This is especially important for people with conditions like fibromyalgia, arthritis, autoimmune disorders, or even unexplained chronic pain. Understanding how your nervous system influences pain can be the missing piece in your healing journey.
Pain Is More Than Just an Injury
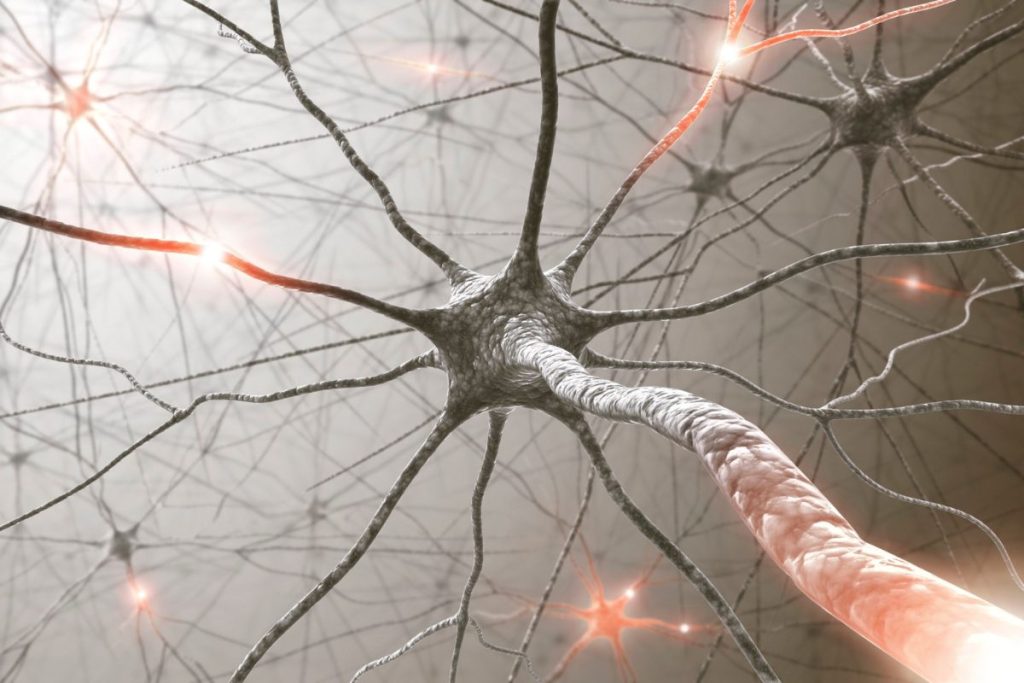
For decades, doctors treated pain as a straightforward message: injury occurs → nerves send signals → brain interprets pain. But research now shows that the brain and nervous system can “turn up the volume” on pain signals.
Dr. Clifford Woolf, a pain researcher at Harvard, explains:
“The nervous system has the capacity to amplify pain, making pain more intense and longer-lasting than would be expected from the initial injury.” (Woolf, 2011, Nature Reviews Neuroscience)
This process, called central sensitization, means your brain and spinal cord essentially become “hyper-alert,” interpreting even normal sensations as painful.
Why the Nervous System Gets Stuck
Several factors can contribute to nervous system hyper-sensitivity:
- Chronic stress – Stress hormones keep the body in fight-or-flight mode, heightening pain signals.
- Inflammation – Systemic inflammation makes nerve endings more reactive.
- Poor sleep – Without restorative sleep, the nervous system can’t reset properly.
- Gut health – Imbalances in the gut microbiome influence inflammation and nerve signaling.
- Hormone imbalances – Cortisol, estrogen, and progesterone shifts can impact how sensitive your nerves are to pain.
Calming the Nervous System to Reduce Pain
Science now shows that the nervous system can be retrained, a process sometimes called pain reprocessing. Just as neuroplasticity allows the brain to learn unhealthy patterns of pain, it also allows it to unlearn them.
Some strategies that research supports include:
- Nutrition for inflammation control – Omega-3s, antioxidants, and nutrient-dense foods reduce neuroinflammation.
- Mind-body practices – Yoga, meditation, and breathwork help calm the amygdala and regulate the stress response.
- Graded movement – Gentle exercise slowly rewires the nervous system to feel safe with movement again.
- Sleep restoration – Deep sleep allows the nervous system to reset and lowers inflammatory chemicals.
- Functional medicine approaches – Addressing hidden infections, toxins, and gut imbalances reduces the triggers that keep the nervous system inflamed

As Dr. Lorimer Moseley, a world-renowned pain scientist, notes:
“We now know that pain is not a measure of tissue damage, but rather an output of the brain designed to protect you.” (Moseley, 2007)
Cindy’s Story: From Fibromyalgia to Freedom
At Wholesome Health, this connection between the nervous system and pain is personal. The founder, Cindy, knows this battle firsthand.
Her journey began with a diagnosis of fibromyalgia, a condition marked by widespread pain, fatigue, and inflammation. For years, she lived with the frustration of doctors offering only temporary relief and little understanding.
Instead of accepting a life defined by pain, Cindy took her health into her own hands. Through functional medicine, nervous system regulation, gut healing, and lifestyle changes, she was able to put her fibromyalgia into remission. Today, she not only feels better than ever but also helps others find freedom from chronic pain.
Moving Forward
At Wholesome Health, we recognize that chronic pain isn’t just about the body, it’s about the nervous system, the immune system, and the environment they’re responding to. Through personalized nutrition, gut restoration, hormone balance, and nervous system support, it is possible to calm inflammation and retrain the brain away from constant pain.
If you’ve been struggling with pain that doesn’t seem to have answers, know that your body is not broken, it’s sending signals that can be rebalanced. Healing is possible when we address the root causes.
👉 Learn more about our Pain & Inflammation Services

References
- Clauw, D. J., Häuser, W., Cohen, S. P., & Fitzcharles, M.-A. (2020). Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain, 161(4), 825–827. https://doi.org/10.1097/j.pain.0000000000001918
- Latremolière, A., & Woolf, C. J. (2009). Central sensitization: A generator of pain hypersensitivity by central neural plasticity. The Journal of Pain, 10(9), 895–926. https://doi.org/10.1016/j.jpain.2009.06.012
- Moseley, L. (2007). Reconceptualising pain according to modern pain science. Physical Therapy Reviews, 12(3), 169–178. https://doi.org/10.1179/174328807X204229
- Woolf, C. J. (2011). Central sensitization: Implications for the diagnosis and treatment of pain. Nature Reviews Neuroscience, 12(11), 695–708. https://doi.org/10.1038/nrn3119
